Cardiology at GM group of hospitals is a state-of-the-art, world class service providing all non-invasive and invasive treatments including open heart surgery.
Both of our hospitals are equipped with a modern cardiac catheter laboratory suite (2 Cath Labs) with all ancillary facilities such as IABP, IVUS for advanced intra vascular ultra-sound imaging, FFR and OCT (Optical Coherence Tomography).
Our non-invasive lab is equipped with the latest in Echocardiography; TMT; Modern Wireless Holter Monitoring; Trans-Esophageal Echocardiography including 3D Echocardiography, Etc. Our Faculty are Key Opinion leaders (KOL) in the field (national experts) with extensive experience both within India and abroad.
We pride ourselves as the most modern cardiac unit in the city of Bangalore with the best, highly qualified and phenomenally experienced Cardiologists providing a personalised care around the clock. All our non-invasive and invasive services are provided at both sites at the most affordable price.
We provide the following invasive cardiac services
Fill-in your details here and our team will get in touch with you shortly.
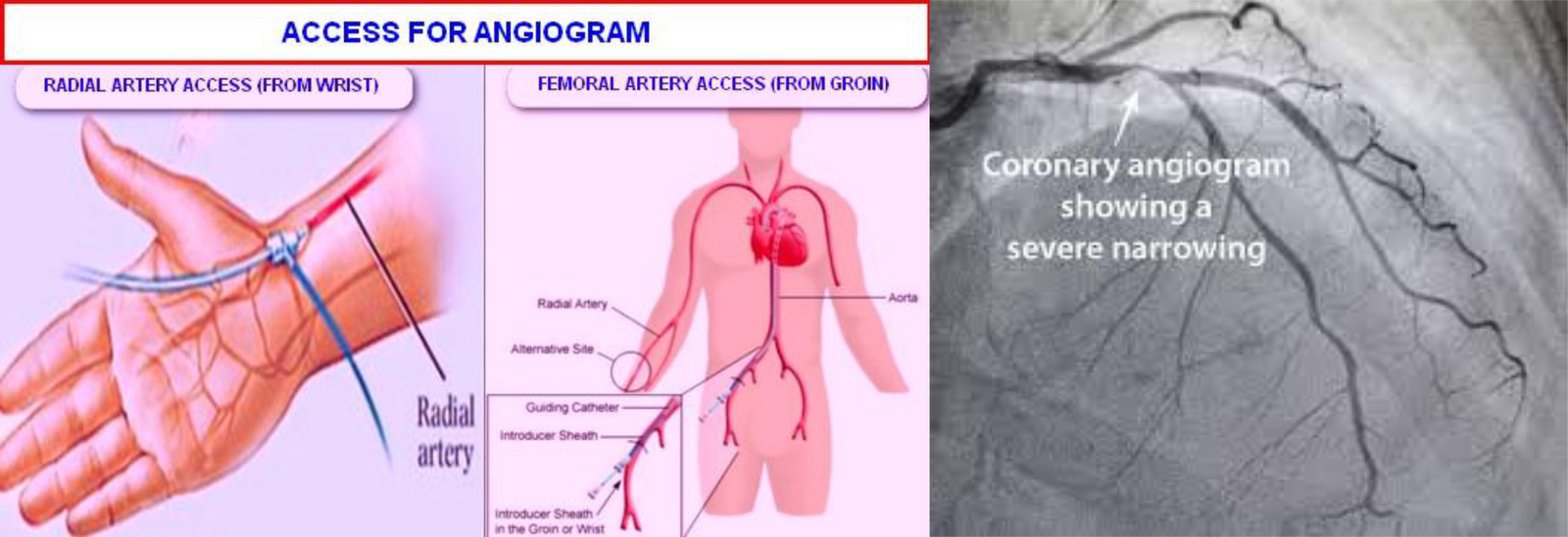
A coronary angiogram (CAG) is the most common invasive procedure done by any interventional cardiologist. This procedure uses X-ray imaging to see your heart’s blood vessels. The test is generally done to see if there’s a narrowing or blockage in the artery that supplies blood to your heart.
During a coronary angiogram, a type of dye that’s visible by an X-ray machine is injected into the blood vessels of your heart. The X-ray machine rapidly takes a series of cine loop x-ray images (angiograms), offering a look at your blood vessels. This is purely a diagnostic test to identify narrowings or blockages.
Once identified, you may be recommended any of the 3 options
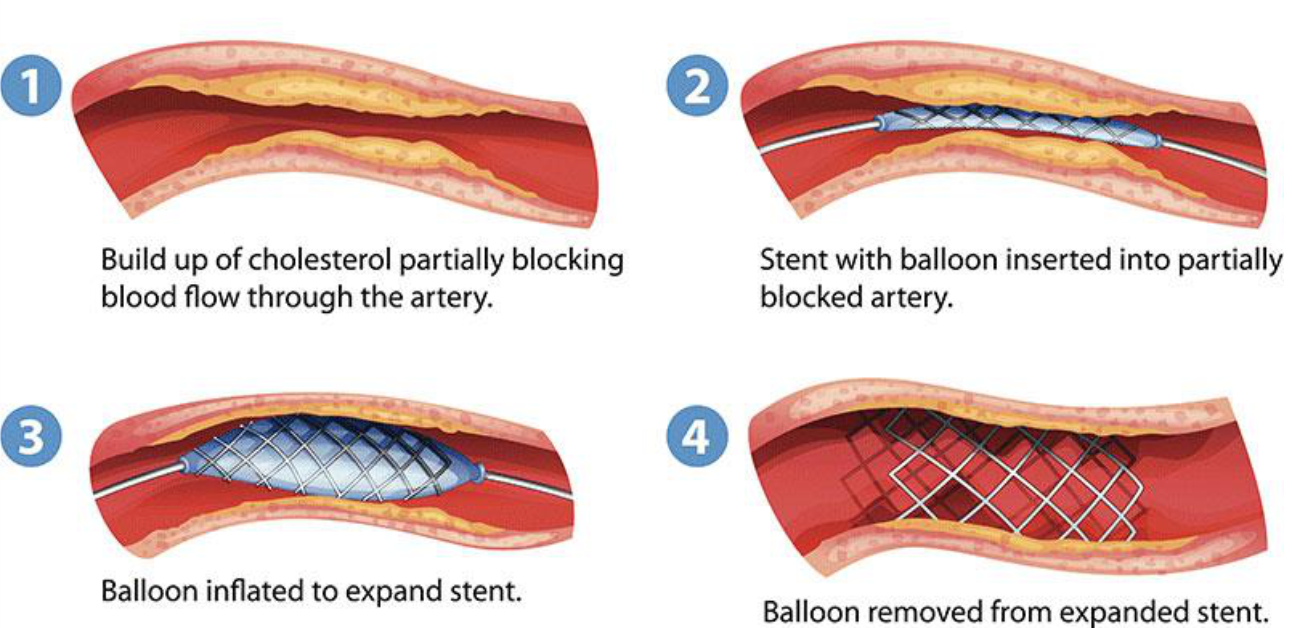
Coronary Angioplasty, also called percutaneous coronary intervention, is a procedure used to open clogged heart arteries. Angioplasty uses a tiny balloon catheter that is inserted in a blocked blood vessel to help widen it and improve blood flow to the heart.
Angioplasty is often combined with the placement of a small wire mesh tube called a stent. The stent helps prop the artery open, decreasing its chance of narrowing again. Most stents are coated with medication to help keep the artery open (drug-eluting stents). Rarely, bare-metal stents are used.
Angioplasty can improve symptoms of blocked arteries, such as chest pain and shortness of breath. Angioplasty is also often used during a heart attack to quickly open a blocked artery and reduce the amount of damage to the heart.
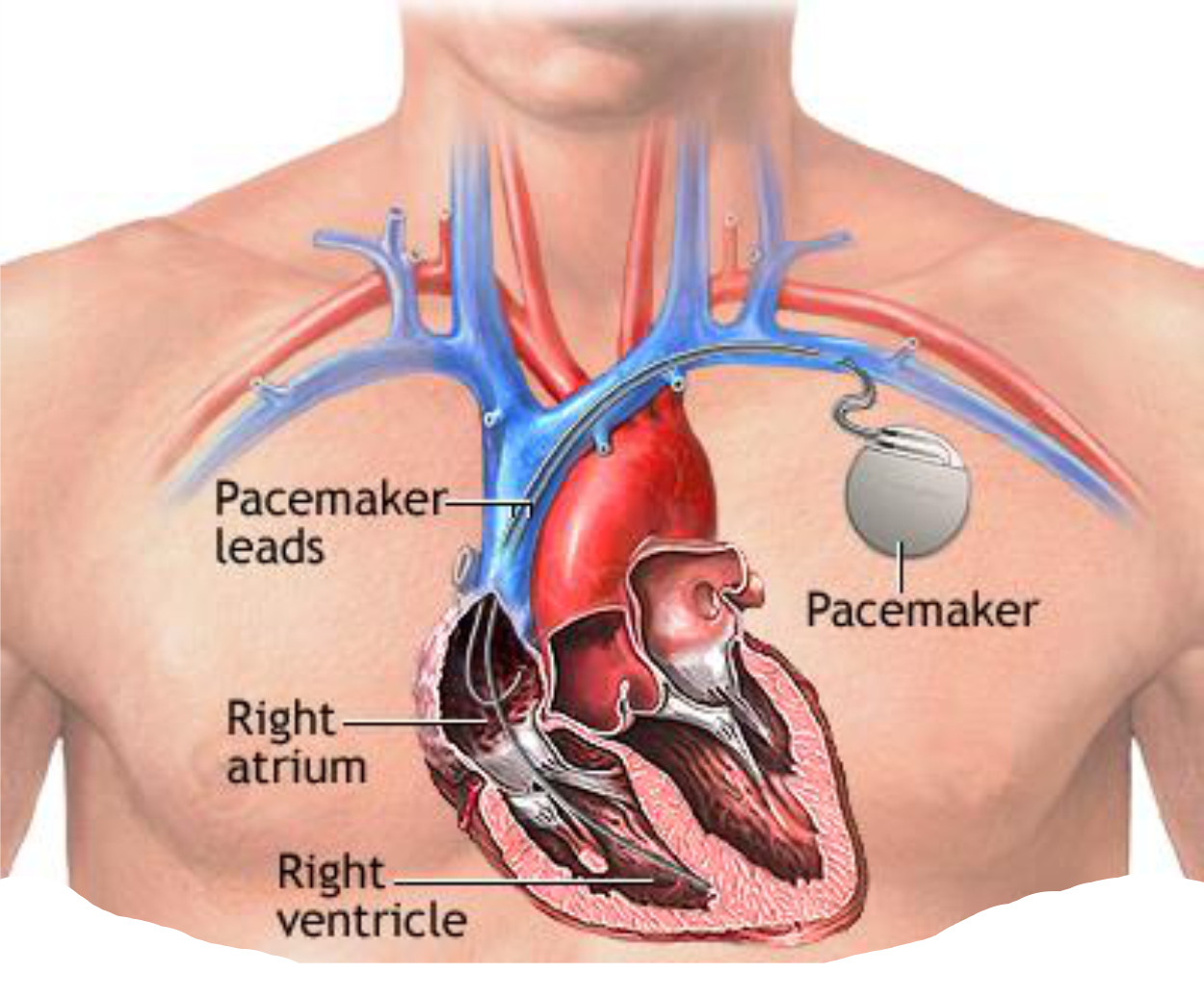
A pacemaker is a small device that’s placed in the chest (or abdomen for infants and children) to treat abnormally slow heart rhythms called bradycardia. This device uses electrical pulses to prompt the heart to beat at a normal rate.
During an episode of bradycardia, the heart may not be able to pump enough blood to the body. This can cause symptoms such as fatigue (tiredness), shortness of breath, or fainting (collapse episodes). Severe and prolonged bradycardia arrhythmias can damage the body’s vital organs and may even cause loss of consciousness or death.
A pacemaker can relieve symptoms of bradycardia such as fatigue and fainting. It will prevent loss of consciousness and fatality due to slow heartbeats and enable the affected person to resume a more active lifestyle.
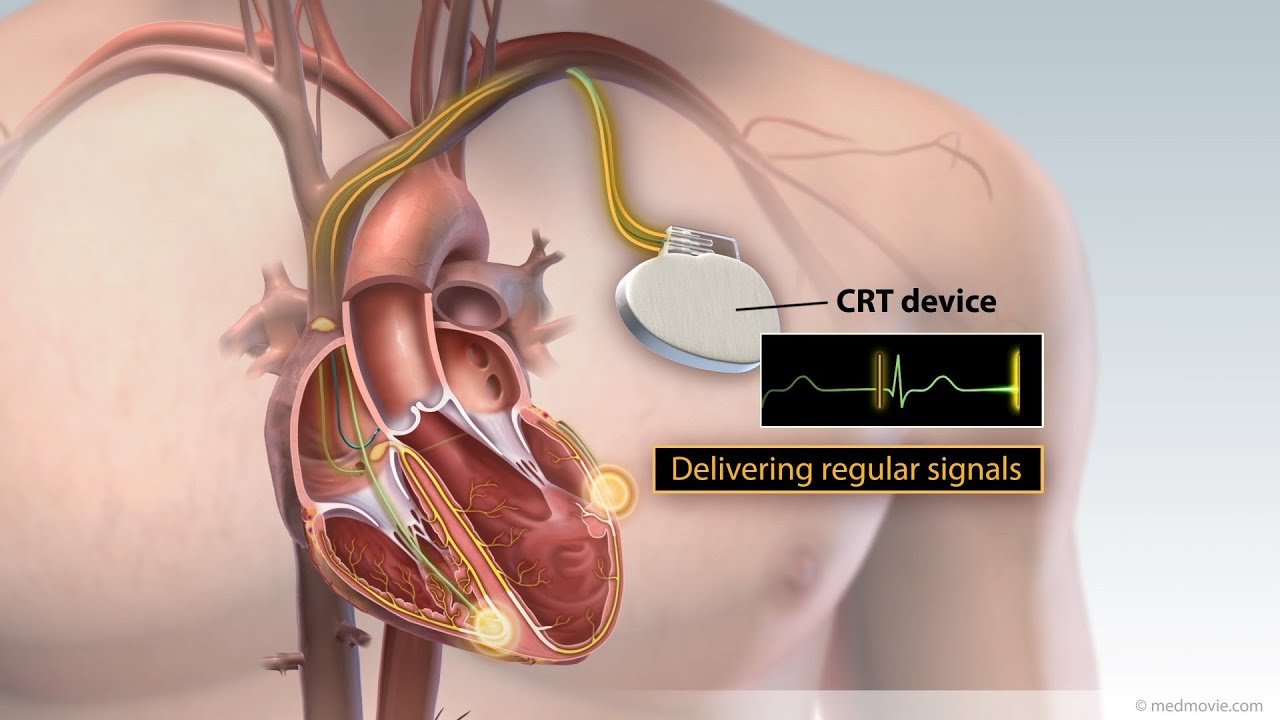
If you are diagnosed with heart failure with reduced ejection fraction (a weak heart) it would help to have a careful look at your ECG to see if you have a condition called Left Bundle Brach Block (LBBB). If you had both, you will benefit from cardiac resynchronization therapy (CRT).
LBBB and heart failure are a common combination. When LBBB co-exists with HF, it makes the weak heart beat in an asynchronous fashion thus making it even more in-efficient. By reversing the electrical phenomenon of LBBB by means of implanting a special pacemaker device with 3 wires (A Bi-Ventricular Pacemaker) the electrical activation of the heart can be made more synchronous (re-synchronisation) which then will make the mechanical function of the heart improve over a period of time.
The procedure involves implanting a pacemaker (the size of 3 ten-rupee coins) just below the collarbone. Three wires (leads) connected to the device monitor the heart rate to detect the heart’s own rhythm and deliver carefully timed electrical impulses to make the heart rhythm more organized.

An automated implantable cardioverter-defibrillator (ICD) is a device that detects any life-threatening, rapid heartbeat termed Ventricular Tachycardia (VT) or Ventricular Fibrillation (VF) and quickly tied to convert it to a normal rhythm by sending some electrical impulses faster that the abnormal heart beat termed Anti-Tachycardia Pacing (ATP) or if that fails, will deliver an electric shock to reset your heart to normal rhythm; A process that is termed DC Cardioversion or defibrillation.
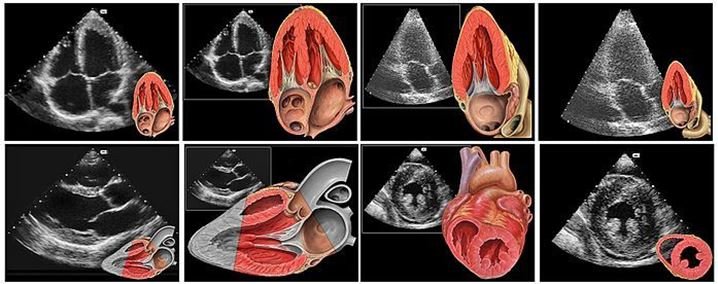
The purpose of this study is to determine the size of your heart, to evaluate how well your heart is functioning or pumping, and to assess the structure and function of the valves within the heart.
A 2D (or two-dimensional) echocardiogram is capable of displaying a cross-sectional “slice” of the beating heart, including the chambers, valves and the major blood vessels that exit from the left and right ventricle. A Doppler echocardiogram measures the speed and direction of the blood flow within the heart. It screens the four valves for leaks and other abnormalities.
By assigning color to the direction of blood flow, (color flow mapping), large areas of blood flow may be studied. These color flow mappings allow abnormal blood flow characteristics to be interpreted by the cardiologist.

Sports cardiology is an advancing field that encompasses the care of athletes and active individuals with known or previously undiagnosed cardiovascular conditions. It incorporates many aspects of cardiology, such as cardiac imaging, electrophysiology, structural heart disease and exercise physiology.
In addition to having training in heart disease (cardiology), doctors in sports cardiology require special expertise and understanding of the physical demands of competitive sports and the psychology of athletes. Our sports cardiologists have training in cardiology and exercise physiology. Sports cardiologists at GM Hospitals also have extensive experience treating athletes with cardiovascular conditions. They also have experience with athletic participation and understand the importance of sports participation to athletes.

A Treadmill (TMT) test, also known as a cardiac stress test, determines how much further your heart can run before developing an irregular beat or blood supply to the heart muscle. It allows your doctor to see how your heart reacts when pressed. You’ll be required to walk or run, with the level of difficulty steadily increasing.

Cardiac rehabilitation, also called cardiac rehab, is a customized outpatient program of exercise and education. The program is designed to help you improve your health and recover from a heart attack, other forms of heart disease or surgery to treat heart disease.
Cardiac rehabilitation often involves exercise training, emotional support and education about lifestyle changes to reduce your heart disease risk, such as eating a heart-healthy diet, maintaining a healthy weight and quitting smoking.
The goals of cardiac rehabilitation include establishing a plan to help you regain strength, prevent your condition from worsening, reduce your risk of future heart problems, and improve your health and quality of life.
Research has found that cardiac rehabilitation programs can reduce your risk of death from heart disease and reduce your risk of future heart problems.
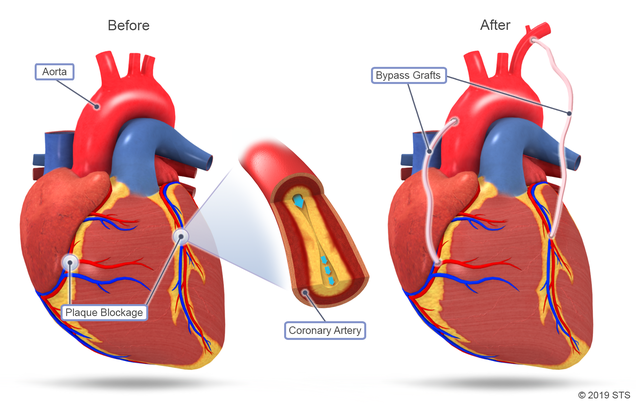
Coronary Artery Bypass Graft Surgery (CABG) is a procedure used to treat coronary artery disease. Coronary artery disease (CAD) is the narrowing of the coronary arteries – the blood vessels that supply oxygen and nutrients to the heart muscle. CAD is caused by a build-up of fatty material within the walls of the arteries.
One way to treat the blocked or narrowed arteries is to bypass the blocked portion of the coronary artery with a piece of a healthy blood vessel from elsewhere in your body. Blood vessels, or grafts, used for the bypass procedure may be pieces of a vein from your leg or an artery in your chest. An artery from your wrist may also be used. Your doctor attaches one end of the graft above the blockage and the other end below the blockage. Blood bypasses the blockage by going through the new graft to reach the heart muscle. This is called coronary artery bypass surgery.
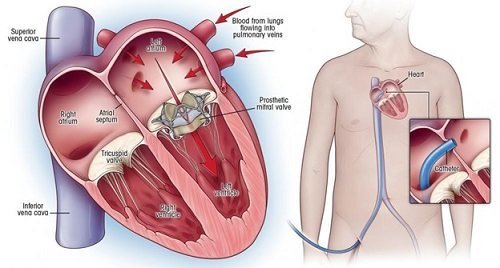
Heart valve surgery is a procedure to treat heart valve disease. Heart valve disease involves at least one of the four heart valves not working properly. Heart valves keep blood flowing in the correct direction through the heart.
The four heart valves are the mitral valve, tricuspid valve, pulmonary valve and aortic valve. Each valve has flaps — called leaflets for the mitral and tricuspid valves and cusps for the aortic and pulmonary valves. These flaps should open and close once during each heartbeat. Valves that don’t open or close properly disrupt blood flow through the heart to the body.
In heart valve surgery, a surgeon repairs or replaces the damaged or diseased heart valve or valves. Many surgical approaches can be used to repair or replace heart valves, including open-heart surgery or minimally invasive heart surgery.
The type of heart valve surgery needed depends on various factors, including your age, your health, and the type and severity of heart valve disease.
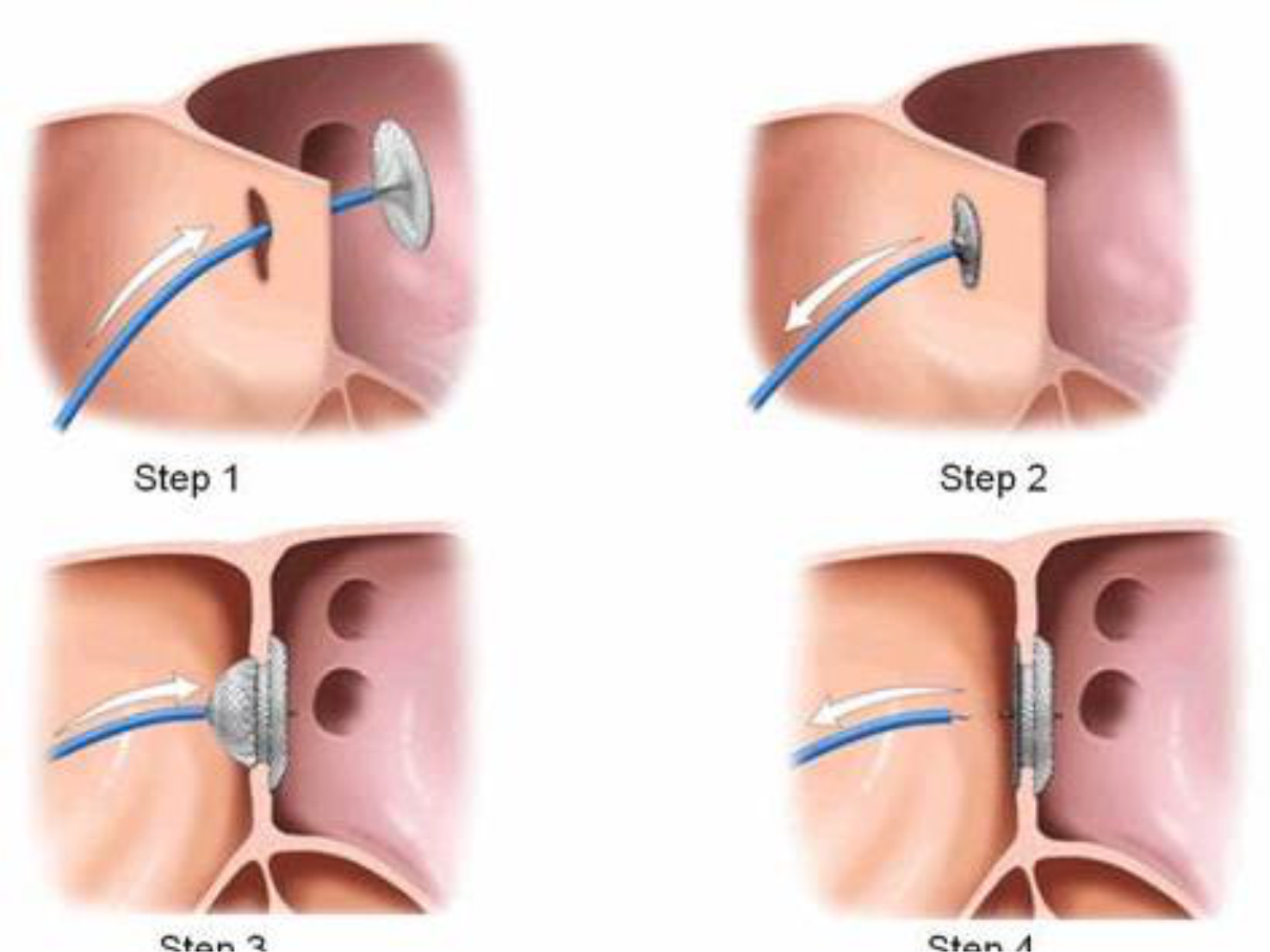
Some children are born with a heart condition called a septal defect. This means there’s a hole in the wall that separates the heart’s four chambers. While this can be a scary diagnosis for any parent to hear, it’s important to keep in mind that the condition is treatable.
An atrial septal defect (ASD) is a hole in the wall between the heart’s two upper chambers. ASD is a congenital condition, which means it is present at birth.
A ventricular septal defect (VSD) is a hole in the wall between the two lower chambers. In children, a VSD is usually congenital.
A septal defect doesn’t always need treatment. If the hole is small and not causing serious symptoms or lowering a child’s quality of life, it can simply be monitored over time. Septal defects can also close on their own as a child grows. “This will usually happen if the defect is located in the part of the septum that’s all muscle,” Barnes adds.
If a hole hasn’t closed on its own within a child’s first two years, or if the hole is larger than 8-10mm, surgery may be necessary. If large holes aren’t closed, there can be long-term consequences from damage to the lungs.
The most common procedures for a septal defect are transcatheter repair and open-heart surgery.
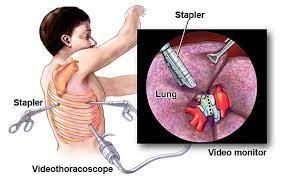
Thoracic surgery can include a variety of operations in your chest (thorax). In addition to your heart and lungs, thoracic surgery can involve your esophagus, trachea or other areas. A heart valve repair, lung tumor removal or aneurysm repair in your chest all fall under the thoracic surgery category.